For adults considering bariatric surgery — whether you're overwhelmed by mounting health concerns Learn more about health concerns, tired of failed diets, or worried about surgical risks and long-term results, this guide is for you. Learn more about long-term results. You want clear differences between options (so you can decide with confidence), honest trade-offs (no sugarcoating), and a plan that matches your life, goals, and medical needs. Our bariatric team can walk you through each procedure step-by-step, matching evidence and real-world experience to your situation so you don't have to guess which bariatric surgery type is the right fit.
What are the main bariatric surgery types?
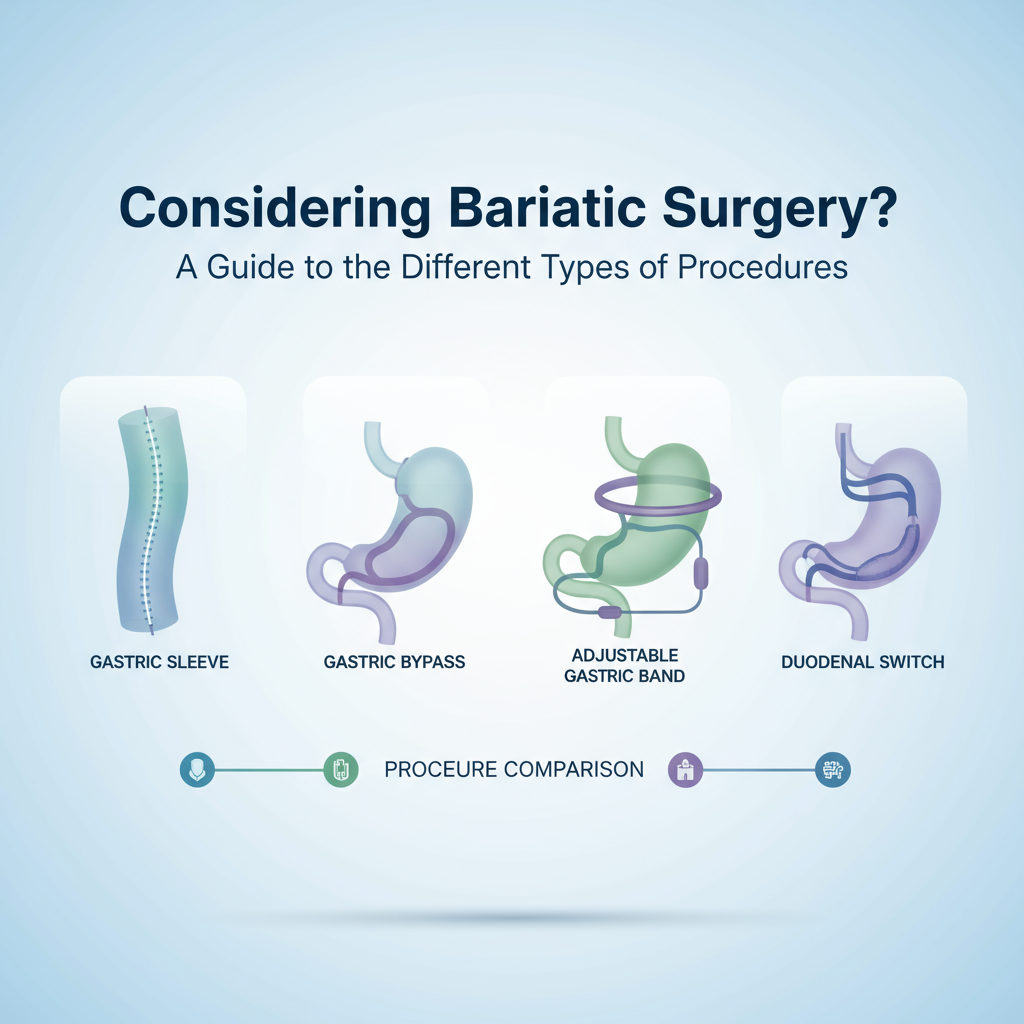
There are four primary bariatric procedures people search for: gastric sleeve, gastric bypass (Roux-en-Y), adjustable gastric band, and duodenal switch (also called biliopancreatic diversion with duodenal switch). Each one changes digestion and appetite in different ways — some reduce stomach volume, others add malabsorption — and that difference matters for weight loss, complications, and lifestyle after surgery.
Gastric sleeve (sleeve gastrectomy) — what it is and how it works
Gastric sleeve removes roughly 80% of the stomach, leaving a narrow “sleeve.” So your stomach holds less food and hormones that drive hunger (like ghrelin) decrease — that’s the twofold effect. It’s done laparoscopically, usually in under 90 minutes.
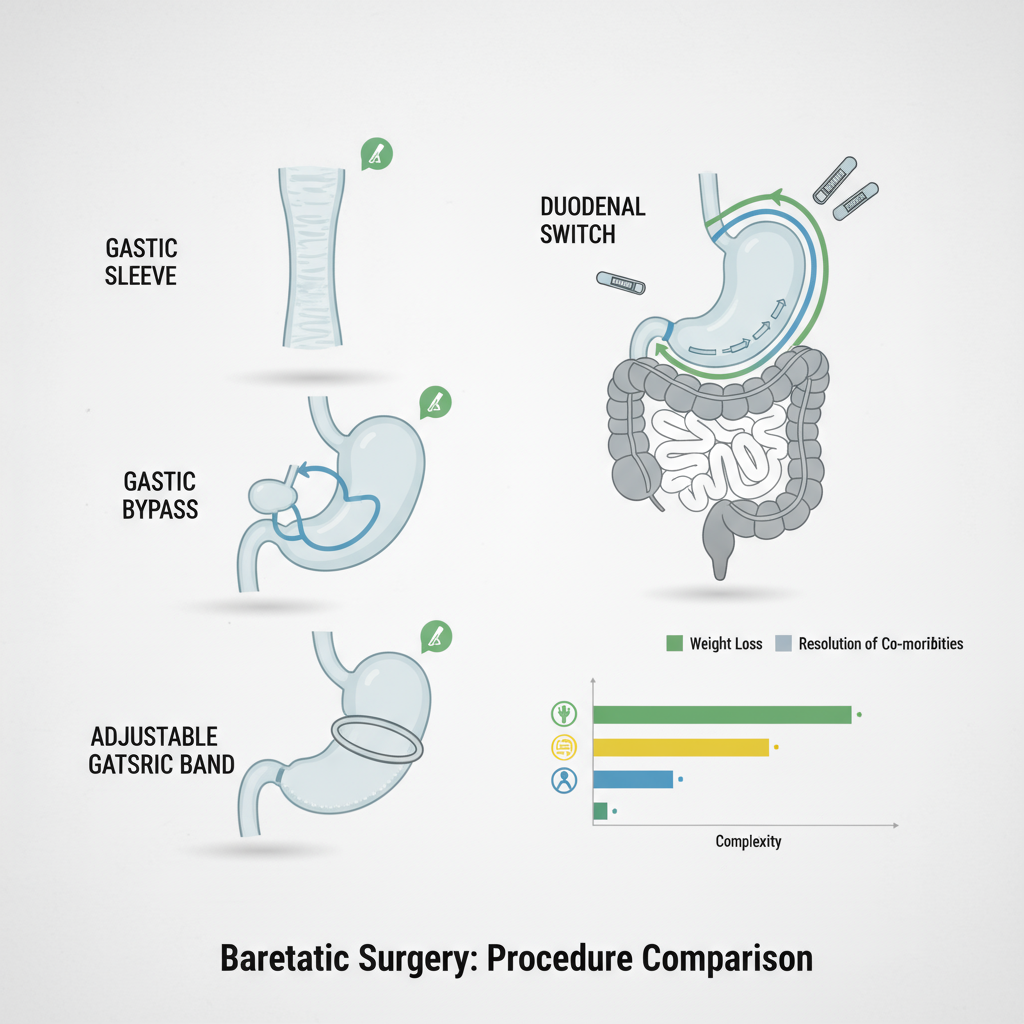
From what I’ve seen, the average excess weight loss is about 65% at 1–2 years post-op. Recovery is typically 2–4 weeks for most people (back to light work sooner), but nutritional follow-up is lifelong — vitamin B12, iron, and vitamin D need monitoring. Learn more about nutritional follow-up.
Pros: strong weight loss, fewer long-term nutritional deficits than duodenal switch, no intestinal rerouting. Cons: irreversible stomach removal, new or worsened acid reflux for some people (GERD can become a real issue).
Gastric bypass (Roux-en-Y) — what it is and how it works
Gastric bypass creates a small stomach pouch (about 15–30 mL) and connects it directly to the small intestine—bypassing the majority of the stomach and the first part of the small intestine. That does two things: you eat less and absorb fewer calories.
In my experience and in the literature, average excess weight loss is near 75% at 1–2 years. It’s often the most predictable for resolving type 2 diabetes quickly (sometimes within days). Recovery is similar to sleeve but nutritional surveillance is more intensive — iron, B12, calcium require monitoring.
Pros: very effective for weight loss and metabolic disease. Cons: higher risk of dumping syndrome (when you eat sugar), more complex surgery and anatomy, slightly higher risk of internal hernias later.
Adjustable gastric band — what it is and how it works
The adjustable gastric band places a silicone ring around the top of the stomach to create a small pouch. The band can be tightened or loosened via a port under the skin (saline adjustments).
I've noticed an average excess weight loss near 40% — and that’s one reason this procedure has fallen out of favor. It’s reversible, and the operation is less invasive, but long-term outcomes include band slippage, erosion, and frequent follow-up for adjustments.
Pros: reversible, lowest immediate surgical risk for some. Cons: long-term device problems are common; weight loss tends to be less and slower; many patients later require removal or revision.
Duodenal switch (biliopancreatic diversion with duodenal switch) — what it is and how it works
This is the most complex: it combines a sleeve-like stomach reduction with rerouting of a large portion of the small intestine to create significant malabsorption. It’s powerful — but so are its consequences.
From what I’ve seen clinically, average excess weight loss is about 85% at 1–2 years. Remission of type 2 diabetes is very high. But long-term nutritional deficiencies (protein, fat-soluble vitamins A, D, E, K) are common — lifelong supplements and close follow-up are mandatory.
Pros: greatest and most durable weight loss, excellent diabetes control. Cons: highest malabsorption risk, more complex surgery, stricter lifelong diet and supplements.
How do these bariatric surgery types compare — short answer
So here's the deal — quick comparisons help when you're choosing:
- Best average weight loss: duodenal switch (about 85%).
- Strong balance of effectiveness and simplicity: gastric bypass (about 75%).
- Good effectiveness with fewer absorption issues: gastric sleeve (about 65%).
- Least invasive but least effective long-term: adjustable gastric band (about 40%).
Think of it like choosing between a Ferrari and a bicycle — powerful vs. low-maintenance. The right choice depends on your health, goals, and willingness to follow lifelong nutrition and follow-up.
Who should consider each procedure?
There’s no one-size-fits-all. But some patterns emerge (these are typical clinical considerations, not strict rules):
- Gastric bypass: a strong option if you have type 2 diabetes, severe GERD, or need potent metabolic control.
- Gastric sleeve: a common default — good for people without severe reflux and who want strong weight loss with fewer absorption issues.
- Adjustable band: sometimes offered to patients wanting a reversible option or those not eligible for other surgeries — but expect more follow-up and potential revision.
- Duodenal switch: for patients with BMI over 50 or significant metabolic disease who prioritize maximal weight loss and accept strict lifelong supplement requirements.
Risks, complications, and what to expect after surgery
All surgeries carry risk — bleeding, infection, anesthesia complications. Specific risks vary by procedure: leaks and strictures can occur after sleeve or bypass, dumping syndrome after bypass, band erosion with adjustable bands, and severe nutrient deficiencies after duodenal switch.
You'll need long-term follow-up — think yearly labs forever. That’s not optional. I've seen good outcomes when patients stick to follow-up and supplement regimens; poor outcomes when they fall out of care.
Common post-op side effects and tips
- Nausea and early satiety — common in the first weeks; start with clear liquids and progress slowly.
- Protein intake — aim for 60–80 grams daily (or as your team prescribes) to prevent muscle loss.
- Supplements — multivitamin plus targeted B12, iron, calcium, vitamin D (dosages vary by procedure).
- Dumping syndrome — avoid high-sugar foods if you have gastric bypass; symptoms include sweating, palpitations, diarrhea after sweets.
Pre-op evaluation and preparation — how to get ready
Expect a multi-disciplinary workup: medical clearance, cardiopulmonary evaluation if needed, nutritional counseling, and psychological screening (this reduces post-op complications). Many centers require supervised weight loss or diet counseling before surgery — not just bureaucracy, but it improves outcomes.
Now, if you’ve been putting off these appointments — get them scheduled. Seriously. Momentum helps. Our team (if you want help) can coordinate these evaluations so you don’t miss anything critical.
How to decide: step-by-step bariatric procedure comparison checklist
Here’s a practical checklist you can use during consults (print it, bring it):
- List your top 3 medical goals (weight loss, diabetes remission, reduced medications).
- Note any digestive issues (GERD, prior ulcers) — these change recommendations.
- Ask the surgeon: expected excess weight loss percentage and complication rates for your profile.
- Ask the dietitian: what lifelong supplements and lab monitoring will be required.
- Clarify follow-up schedule and who performs revisions if needed.
- Compare recovery time and return-to-work expectations (you’ll want specifics for your job).
Real-world outcomes — what patients actually report
I've noticed two things: first, patients who commit to follow-up and lifestyle changes get better long-term results; second, surgical skill and team support matter a lot — not just the type of procedure. Weight loss percentages are averages, but your individual effort and the post-op program (nutrition, exercise, behavioral health) shape long-term success.
When to consider revision surgery
Some patients need a second operation — for inadequate weight loss, weight regain, or complications (like band erosion). Gastric band patients have the highest revision rate historically; conversions to sleeve or bypass are common. If you're worried about future revisions, ask your surgeon about durability stats for your specific case.
Questions to bring to your surgeon
- How many of this type of surgery does your team perform per year?
- What are my personalized expected weight-loss numbers and complication risks?
- What exactly will my supplement and lab schedule look like?
- Who provides long-term follow-up and how do I access support (dietitian, psychologist)?
Choosing the right center — what to look for
Pick a center with a multidisciplinary team (surgeon, dietitian, psychologist, primary care coordination) and transparent outcomes data. Visit support groups (virtual or local) — you'll learn fast. And ask about emergency protocols — complications sometimes present after hours.
Final thoughts — balancing risk, lifestyle, and goals
Choosing a bariatric surgery type is a trade-off: more weight loss usually means more long-term nutritional vigilance. That's the truth. If you're aiming for maximum diabetes control and weight loss and you're prepared for strict follow-up, duodenal switch might fit. If you want strong results with somewhat simpler nutrition, gastric bypass or sleeve are often better. If reversibility is your top priority — adjustible band — but be realistic about outcomes.
If this feels overwhelming, our team can handle the details for you — coordinating evaluations, explaining lab results, and mapping a lifelong follow-up plan so you can focus on recovery and new habits.
FAQs
Which bariatric surgery is best for type 2 diabetes?
Gastric bypass and duodenal switch have the highest rates of diabetes remission — gastric bypass works quickly and predictably for many patients (I’ve seen medications stop within days in some cases). Duodenal switch often gives the most durable control but demands stricter follow-up and supplements.
Will I regain weight after bariatric surgery?
Some weight regain is common over years, especially if follow-up care and lifestyle changes lapse. The procedures with the highest long-term weight maintenance tend to be duodenal switch and gastric bypass; adjustable band sees the highest rates of weight regain. Regular follow-up, exercise, and nutrition are key to minimizing regain.
How long is recovery after bariatric surgery?
Most people return to desk work in 2–4 weeks. Full recovery (exercise, heavier activity) is usually 6–8 weeks, depending on procedure and personal healing. Your surgeon will give a tailored timeline.
Do bariatric surgeries affect pregnancy?
Yes — pregnancy is generally discouraged for 12–18 months after surgery while weight stabilizes, and vitamin monitoring during pregnancy is essential. But many patients have safer pregnancies post-weight-loss surgery because weight-related risks decrease.
How do I start the evaluation process?
Begin with your primary care doctor or contact a bariatric center to schedule a consult. Expect labs, nutritional and psychological screening, and education sessions. If you'd like, we can help coordinate those first appointments and give you a checklist to bring to your consult.