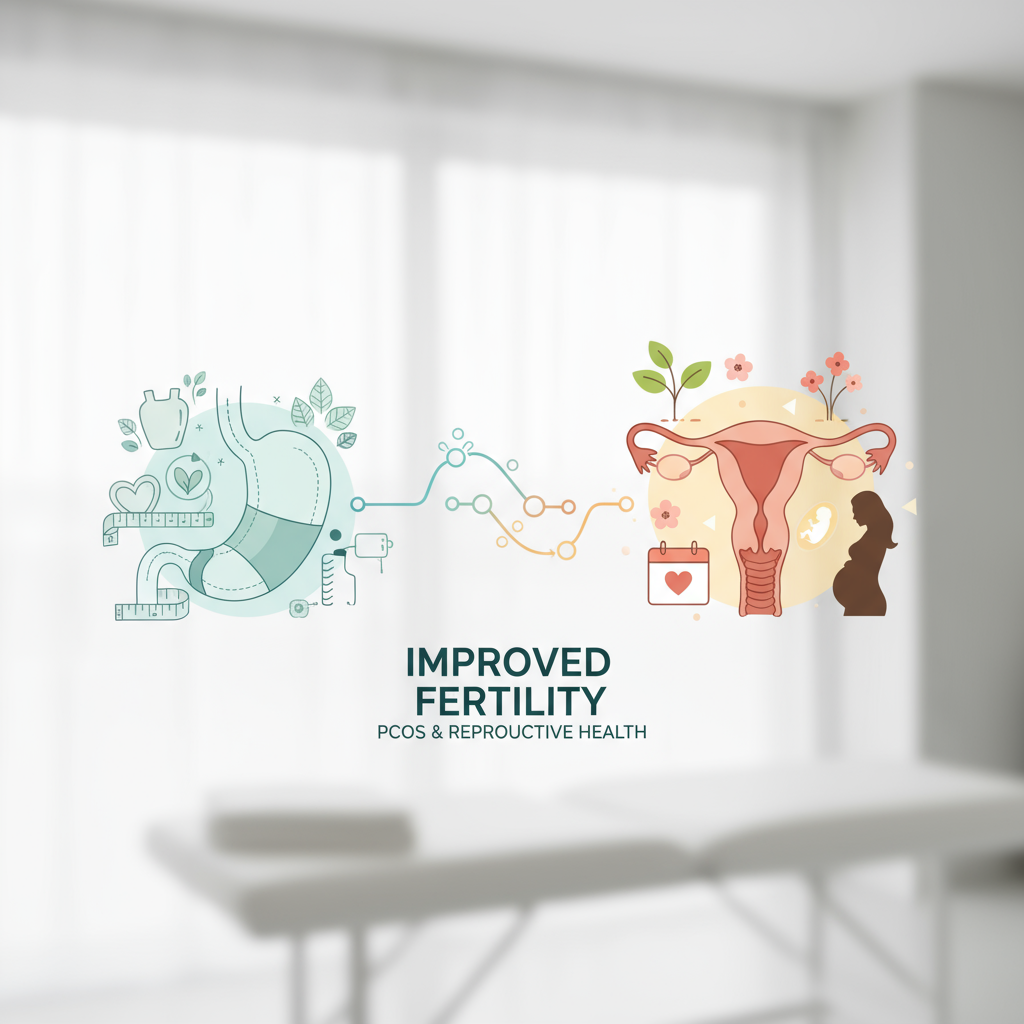
Exploring the Link Between Bariatric Surgery and Improved Fertility
This is for people trying to conceive who are also dealing with obesity, PCOS, irregular cycles, or frustrating “unexplained” infertility that doesn’t feel so unexplained anymore. You want answers, you’re tired of meds that don’t stick, and you’re worried that time is slipping by while your body won’t cooperate—especially if cycles are all over the place or you’ve been told to “just lose weight” (not helpful). Our bariatric and reproductive health team guides patients through evidence-based weight loss surgery options, fertility-safe timelines, and nutrition plans so you can improve reproductive health and move toward a healthy pregnancy without guesswork. Learn more about nutrition plans. Learn more about successful long-term health.
Does bariatric surgery improve fertility?
Yes—weight loss after bariatric surgery is linked to better ovulation, more regular periods, and higher natural conception rates, especially in people with PCOS. Why? Because fat tissue isn’t just storage; it’s hormonally active. Losing significant weight reduces insulin resistance and androgen excess, helping the brain–ovary axis fire properly again. I’ve seen patients go from 45–60 day cycles to 28–32 days within a few months, and that shift alone can change everything.
There’s more. Pregnancy after bariatric surgery often carries lower risks of gestational diabetes and hypertensive disorders compared with pregnancies at higher BMIs without surgery. Learn more about other health improvements. But it’s not a free pass—nutrient deficiencies can creep in if you don’t plan ahead. Learn more about nutrient deficiencies. So we pair the upside with tight nutrition and lab monitoring.
How does weight loss surgery affect PCOS and ovulation?
PCOS and bariatric surgery have a unique synergy. Reduced insulin levels lower ovarian androgen production, which helps follicles mature and ovulation resume. Many patients notice:
- Cycle regularity returning within 3–6 months
- Improved acne and hirsutism (not overnight—but real changes)
- Improved response to fertility meds if they’re still needed
In my experience, cycle tracking often becomes useful again—LH surges show up, basal body temps stabilize, and ovulation predictor kits stop feeling like a scam.
How soon can pregnancy happen after bariatric surgery?
Fertility can rebound quickly—sometimes too quickly. That’s why most guidelines advise avoiding pregnancy for 12–18 months after surgery while weight stabilizes. Contraception matters here (IUDs or implants are great choices). The goal: enter pregnancy with stable weight, optimized nutrients, and a clear plan.
How much weight loss improves fertility?
Even a 5–10% body weight reduction can improve ovulation in PCOS. After bariatric surgery, patients often lose much more, which amplifies hormonal benefits. No magic number exists, but restored regular cycles are a strong signal you’re on the right track.
Is pregnancy after bariatric surgery safe?
It can be very safe—and often safer than pregnancy with untreated obesity—if you plan it. There are two sides to the coin: reduced risks from weight loss, and new considerations from surgery.
What are the risks and how do you manage them?
- Nutrient deficiencies (iron, B12, folate, vitamin D, calcium; fat-soluble vitamins with malabsorptive procedures). Fix with targeted supplements and routine labs.
- Small-for-gestational-age (SGA) infants. Balanced calorie and protein intake helps—no crash dieting during pregnancy.
- Dumping syndrome or hypoglycemia after gastric bypass. Smart meal timing and low–simple sugar eating keep glucose steady.
- Internal hernia risk after bypass—new abdominal pain in pregnancy needs quick surgical evaluation. Don’t wait it out.
- Gallstones from rapid weight loss—watch for right-upper-quadrant pain; treat early.
Real talk: you want a bariatric-aware OB team. We coordinate care so your prenatal visits include nutrition, labs, and a watchful eye on weight trends that make sense post-surgery, not generic targets.
What prenatal vitamins and labs are recommended after bariatric surgery?
Baseline before trying to conceive, then once each trimester (and more often if abnormal):
- Complete blood count, ferritin/iron studies
- Vitamin B12, folate
- Vitamin D, calcium, PTH
- Fat-soluble vitamins (A as beta-carotene preferred, E, K) if malabsorptive procedure
- Thiamine if prolonged vomiting
- Albumin/prealbumin for protein status
Supplement game plan most patients use:
- High-quality prenatal with at least 800–1,000 mcg folic acid (5 mg if high risk—history of NTDs, certain meds—ask your clinician)
- Iron 45–60 mg elemental daily (separate from calcium)
- Vitamin B12 350–500 mcg daily orally or 1,000 mcg monthly IM if levels lag
- Calcium citrate 1,200–1,500 mg daily in divided doses + vitamin D3 2,000 IU (adjust to labs)
- Protein: aim 60–80 g daily, often higher by trimester 2–3
- Vitamin A as beta-carotene only—avoid high-dose retinol in pregnancy
And hydrate. Sounds basic, but dehydration drives nausea and constipation, which then mess with intake… you get the idea.
How is gestational diabetes screened after bariatric surgery?
Standard oral glucose tolerance tests can trigger dumping and give misleading results after bypass or sleeve. Many clinicians use home glucose monitoring instead: fasting and 1-hour postprandial checks for 1–2 weeks around 24–28 weeks. It’s practical and patient-friendly.
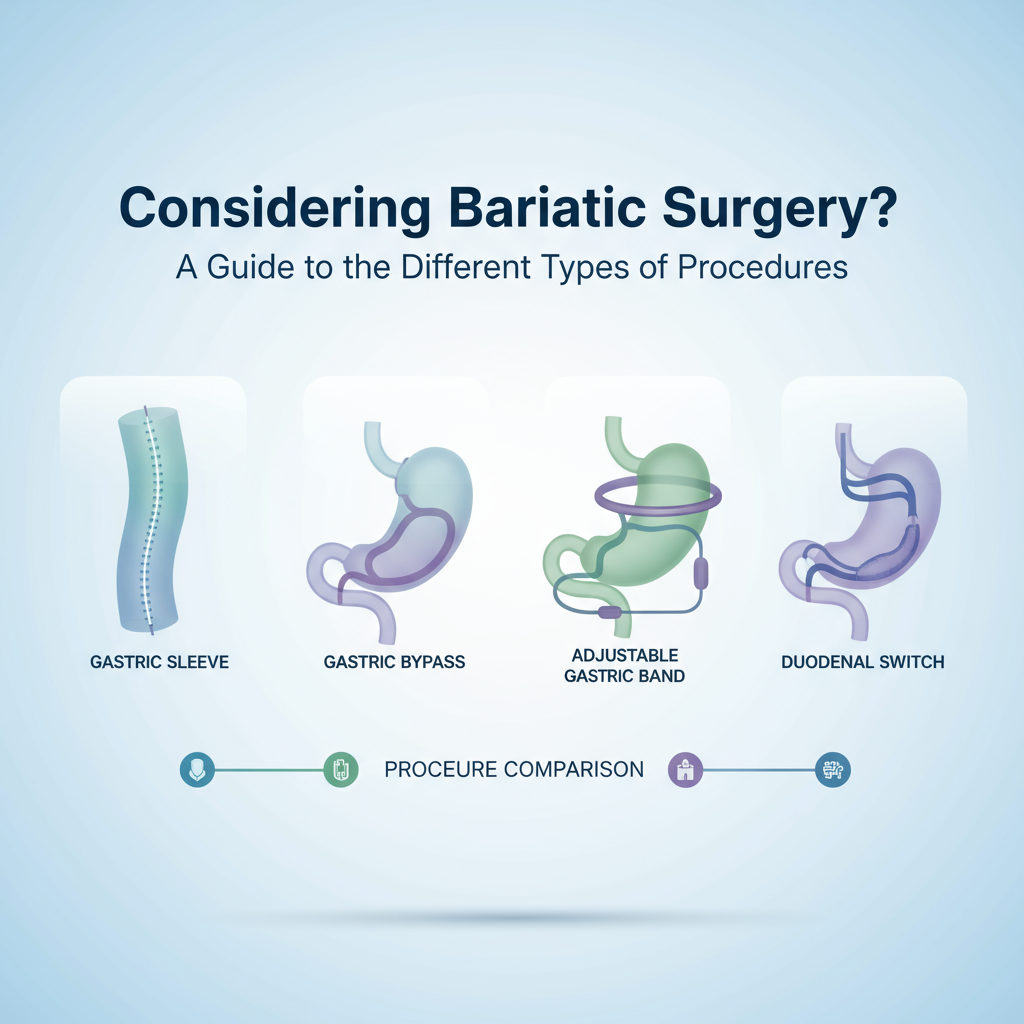
Which bariatric procedure is best for fertility goals?
There’s no one-size-fits-all. Sleeve gastrectomy and gastric bypass both improve fertility and PCOS symptoms. Sleeve: fewer malabsorption issues, simpler supplementation. Bypass: strong metabolic impact for insulin resistance but higher internal hernia and deficiency risks. Duodenal switch has powerful weight loss but the highest deficiency burden—usually not a first choice if near-term pregnancy is a priority.

Look, it’s like choosing between a Ferrari and a bicycle—except it isn’t. It’s more like choosing between two reliable SUVs with different maintenance plans. We map your medical history, BMI, reflux, diabetes status, and fertility timeline to pick the right tool.
Does bariatric surgery improve male fertility?
Often, yes. Weight loss can improve testosterone, reduce estrogen from adipose conversion, and enhance sperm parameters. I’ve watched couples move from borderline semen analyses to normal counts within months of steady loss. That said, extreme calorie deficits can temporarily dip testosterone, so slow-and-steady nutrition still wins.
How to plan pregnancy after bariatric surgery: a simple checklist
- Decide on surgery type with both metabolic and fertility goals in mind.
- Use reliable contraception post-op; target pregnancy at 12–18 months when weight stabilizes.
- Start a bariatric-safe prenatal early, then individualize iron, B12, vitamin D, calcium, and others to labs.
- Track cycles—OPKs or temping—to confirm ovulation as weight comes off.
- Meet with a bariatric-aware OB and a dietitian before trying to conceive.
- Plan glucose screening via home monitoring instead of sugar drinks if advised.
- Report new abdominal pain urgently in pregnancy (don’t “push through” possible internal hernia).
- Keep protein up, meals steady, and nausea managed to protect micronutrient intake.
If this feels overwhelming, our team can handle it for you—procedure selection, labs, supplements, and a trimester-by-trimester plan that keeps you and baby well-nourished.
FAQs about fertility and pregnancy after bariatric surgery
How fast can ovulation return after surgery?
Some patients ovulate as early as 4–8 weeks once insulin resistance improves. That’s why contraception from day one matters.
Can I use fertility meds after bariatric surgery?
Yes. In fact, response to letrozole or gonadotropins can improve as weight and insulin resistance come down. Your REI may lower doses compared with pre-op plans.
Will I need a C-section?
Not automatically. Mode of delivery depends on obstetric indications, not the surgery alone.
What if I conceive sooner than 12 months?
Don’t panic. Call your care team quickly, intensify nutrition monitoring, and adjust supplements. Many patients do well with tighter follow-up.
Are there foods I should avoid during pregnancy after bariatric surgery?
Greasy, very sugary, or liquid-calorie foods often trigger dumping or reactive lows. Small, protein-forward meals—think eggs, Greek yogurt, chicken, tofu—tend to sit best.
So here’s the thing about bariatric surgery and fertility—it’s not “weight loss for looks.” It’s metabolic recalibration that can reboot ovulation, tame PCOS, and set you up for a stronger pregnancy journey. If you want a clear, step-by-step path from surgery to safe conception, we’d love to help you map it—no cutting corners, just smart, coordinated care that respects your timeline.