For bariatric patients (sleeve, bypass, or revision) who want a calmer, healthier relationship with food, yet keep bumping into stalls, grazing, or “I’m full… but I still want more”—this guide is for you. You’re juggling satiety cues that feel new, a post-bariatric surgery diet that’s strict, social pressure, and maybe a fear of regain. Learn more about maintaining weight loss. Plus the holidays or football-season tailgates don’t exactly make it easier. Our bariatric nutrition team helps patients turn mindful eating into a practical, non-judgy system—so you can eat with confidence, protect your results, and actually enjoy meals again without white-knuckling it.
What is mindful eating after bariatric surgery?
Mindful eating is paying full attention to your food—how it looks, smells, tastes, and how your body responds—so you stop when your body says “enough,” not when the plate is empty. After bariatric surgery, mindful eating becomes a core tool for bariatric nutrition because your anatomy changed. You have a smaller stomach, faster fullness, and in some cases altered absorption. So the game shifts from volume to presence—slow pace, protein-forward bites, and noticing satiety cues early.
Why mindful eating matters more after sleeve or bypass
Small pouch, big consequences. Eat too fast and you’ll miss early fullness signals, then hit a hard stop (pain, chest pressure, hiccups). Choose “slider foods” and you can overeat without feeling full, which can stall weight loss and energy. Mindful eating helps you meet protein goals, reduce dumping syndrome risk, avoid grazing, and build healthy eating habits you can actually maintain—on a random Tuesday or at your cousin’s wedding buffet. Learn more about building healthy eating habits. Learn more about protect your results.
Mindful eating options: which method fits your style?
There isn’t one “right” mindful eating method. Think of these like tools. You’ll probably mix two or three depending on the day. I’ve seen patients thrive by keeping it simple—no perfection required.
Option 1 — Hunger–Fullness Scale (0–10): Rate your hunger before, during, and after meals. Start eating near 3–4 (pleasant hunger), stop near 6–7 (satisfied, not stuffed). Best for: people who enjoy quick self-checks and like data without logging calories.
Option 2 — The 20–20–20 Method: Take a 20-cent-size bite, chew ~20 times, make the meal last ~20 minutes. It sounds gimmicky, but it slows intake enough for satiety to show up. Best for: fast eaters and anyone who tends to “forget” to pause between bites.
Option 3 — Protein-First Plate: Eat dense protein first (chicken, fish, Greek yogurt, eggs), then non-starchy veggies, then high-fiber carbs if there’s room. Why? Protein drives satiety and supports healing and muscle. Best for: folks who feel full fast and need to prioritize nutrition over volume.
Option 4 — Photo Food Logging vs App Tracking vs Paper Journaling: Photo logging (snap before you eat) improves mindfulness instantly because it inserts a pause. App tracking (like Baritastic) gives protein counts and timing. Paper journaling captures mood, triggers, and satiety cues in your own words. Best for: visual learners (photos), data lovers (apps), deep reflectors (paper). Compare your energy the week you photo-log vs the week you app-track—you’ll know your fit pretty quickly.
Option 5 — Environment Reset: Sit at a table, no screens, smaller plate, fork down between bites, a sip only before and 30 minutes after. It’s basic—yet powerful. Best for: people who “accidentally” speed-eat while working, parenting, or streaming Netflix. And yes, I get it—life is loud—so even 10 quiet minutes counts.
Option 6 — Timer or Bite Counter vs Internal Cues: Some patients use a 20–25 minute timer or a slow-eating device to pace meals. Others rely purely on breath, pauses, and body sensations. Best for: early months (external pacing helps), then gradually shift to internal cues as you gain confidence.
Option 7 — Group Support vs 1:1 Coaching vs Self-Guided: Group sessions add accountability and real-world tips (“What do I order at Chipotle?”). 1:1 support personalizes strategies around your schedule, labs, and triggers. Self-guided works if you’re structured and like experimenting. Best for: different seasons—start with coaching, then maintain with group, then self-guided when routines stick.
Mindful eating vs calorie tracking after bariatric surgery
Short answer: you can do both, but mindful eating does the heavy lifting. Mindful eating helps you notice satiety cues, slow down, and pick protein—those behaviors drive results. Tracking is a tool, not a lifestyle. Use it for 14 days to calibrate protein and fluid, then switch to photo logging or targeted check-ins. Think of tracking like a GPS on a new route; once you know the turns, you don’t need it every day.
How to recognize satiety cues after bariatric surgery
Your cues might be surprisingly subtle. Or oddly specific. I’ve noticed patients report a small sigh, a runny nose, a single hiccup, or gentle pressure below the sternum as the first “soft stop.” That’s your cue to pause for 2–3 minutes. A “hard stop” looks like sharp chest pressure, nausea, or saliva surges—don’t push past that. Respecting the soft stop prevents the hard stop.
Practical steps: Before you eat, rate hunger (0–10). Mid-meal, pause after 5–6 bites; scan for softness in your stomach area. If you feel food stacking up or pressure rising, set the fork down and breathe for 60–90 seconds. If satisfaction holds, you’re done—save it. If genuine hunger is still present, take two slow bites and reassess.
Sample mindful meal flow (about 20–25 minutes)
Minute 0–1: Look at your plate. Name the protein and veggie out loud—yes, literally—because it primes protein-first thinking. Quick gratitude or intention: “Fuel, not stress.”

Minute 1–5: Two tiny bites, chewed well. Notice texture and temperature. Put utensils down between bites. If you’re with family, ask a question, listen fully, then take the next bite—conversation builds natural pauses.
Minute 5–10: Continue protein-first. Sense for soft-stop cues: slight chest warmth, small sigh, slower breathing. If you notice them, take a 90-second pause.
Minute 10–15: If hunger remains, finish protein, then add a few veggie bites. No drinking with meals. If you feel pressure or hiccup, you’re done—even if there’s two bites left. That leftover is future-you’s win.
Minute 15–20: Stop at satisfied (6–7 on the scale). Take a walk or rinse the plate to close the loop. Set a 30-minute timer before any fluids. That gap protects your satiety.
Common pitfalls and quick fixes
Grazing all afternoon: Anchor meals. Plan three protein-forward eating times and one intentional snack. Put food on a plate—standing at the counter doesn’t count.
Slider foods (chips, ice cream, mashed potatoes) overshooting satiety: Pair sliders with a dense protein or swap for Greek yogurt, cottage cheese, or edamame. If it dissolves, it likely won’t satisfy.
Drinking with meals: It speeds food through the pouch. Keep a water bottle in another room during meals, then sip every 10–15 minutes after your 30-minute wait.
Speed eating at work: Schedule 15 minutes on your calendar titled Meeting: Lunch Focus. Sounds silly. Works beautifully.
Social events: Eat a protein snack 30–45 minutes before. At BBQs, start with brisket or chicken, then slaw (vinegar-based). Skip grazing platters unless you’ve plated it.
Stress eating: Two-minute “box breath” before meals (inhale 4, hold 4, exhale 4, hold 4). Or use a meditation app right before dinner—small reset, big payoff.
People Also Ask: fast answers
What can I eat 3 months after bariatric surgery to practice mindful eating?
By month 3, most patients tolerate tender proteins (shredded chicken, flaky fish, turkey meatballs), eggs, Greek yogurt, cottage cheese, tofu, and soft-cooked veggies. Build meals protein-first, then add high-fiber carbs like berries or beans if there’s room. Take small bites, chew well, and stop at the soft cue—don’t chase “just two more.”
Can mindful eating prevent dumping syndrome?
It helps. Mindful eating slows pace and encourages label checks, which reduces big sugar hits and large volumes that trigger dumping. Pair carbohydrates with protein, avoid drinking with meals, and stop at satisfaction. If you’ve had episodes, pre-plan snacks (like 2 ounces of cheese and 6–8 crackers) so you’re not grabbing sweets out of panic.
How many minutes should a post-bariatric meal take?
About 20–25 minutes for most meals, 10–15 for snacks. If you’re done in 6 minutes, you likely ate too fast. Set a gentle timer or try the 20–20–20 method until your natural pace slows.
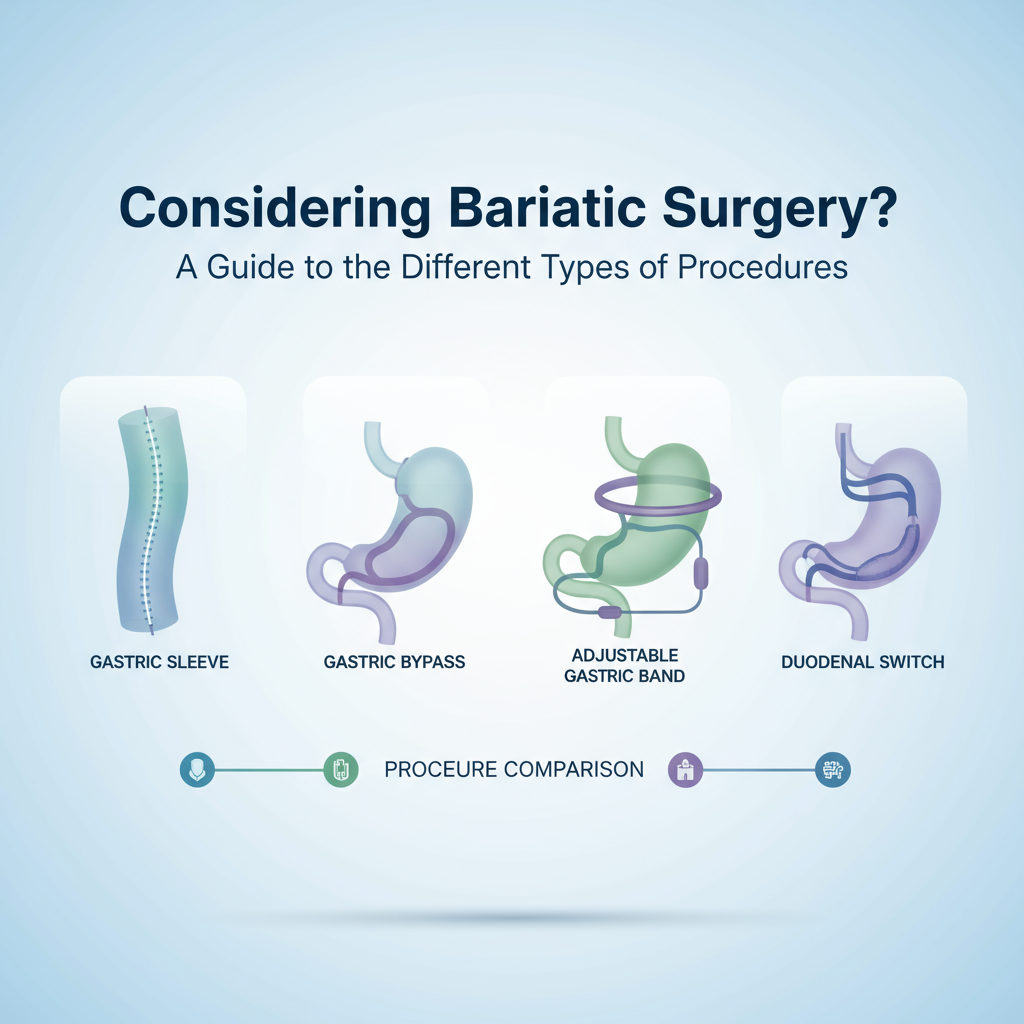
Is mindful eating different after gastric sleeve vs bypass?
The principles are the same, but bypass patients may notice dumping syndrome and reactive hypoglycemia more often, so pacing and protein pairing matter even more. Sleeve patients often report stronger restriction with dense protein—tiny bites and longer chewing help a lot.
Do I need to avoid snacks if I’m eating mindfully?
No. Planned snacks can stabilize energy and protein intake. Aim for protein-forward options (yogurt, jerky, a cheese stick, edamame). The key is intention: sit, plate it, and use the same slow-bite rules.
Mindful eating options compared: choose your starter combo
If you want the lowest-lift start, pair the 20–20–20 method with protein-first plates. You’ll get immediate wins—fuller on less, fewer “hard stop” moments.
If you’re very data-driven, combine the Hunger–Fullness Scale with 14 days of app tracking to nail protein and fluids, then shift to photo logging to keep mindfulness high without the mental load.
If stress is your main barrier, go with Environment Reset plus a 2-minute breath before meals. From what I’ve seen, this combo calms pace better than any gadget—because it addresses the actual trigger.
A realistic day of mindful eating (example)
Breakfast: 5 ounces Greek yogurt with 1 tablespoon peanut powder and 6 raspberries. Small spoon, slow bites, 10 minutes. Soft stop? Save the rest.

Lunch: 3 ounces salmon, 1/2 cup roasted zucchini. 20–20–20 rule. Pause halfway, check satiety cues.
Snack: 1 cheese stick and 1 small apple, eaten separately—protein first, then fruit if still hungry after 5 minutes.
Dinner: 3 ounces chicken taco bowl (chicken, salsa, lettuce, a few beans). No liquids during the meal. Walk 5 minutes after. That’s it—simple, not spartan.
Tools we actually recommend
Baritastic app for protein and hydration tracking in the first 2–4 weeks of a new routine. Ate-style photo journaling for quick mindfulness. A small salad fork and 7-inch plate for natural portion control. A quiet 20-minute timer. And if you like meditation, try a free 5-minute session before dinner—you’ll eat slower without trying.
How to adjust during tricky seasons
Holiday spreads, summer BBQs, big games—tempting. Real talk: plan the protein. Choose one dessert and savor it slowly instead of nibbling at five. Walk between courses. And if you slip? No drama. One choice doesn’t rewrite your progress; your next protein-forward meal does.
Where our team fits in
If this all feels like a lot—because life—our clinicians can personalize a mindful eating plan around your procedure, labs, and schedule. We’ll map your satiety cues, set protein targets that match your body, and build meal rituals that work whether you’re traveling for work or feeding three kids at 7 p.m. If you want, we’ll review a week of photo logs and highlight exactly where to slow down, what to swap, and how to hit protein without feeling deprived. You make the decisions; we make it easier to stick with them.
Bottom line: savor, don’t struggle
Mindful eating is not a diet—it’s your daily driver after bariatric surgery. Start with two small tools (20–20–20 and protein-first), watch for soft-stop cues, and protect your meal environment. The simplicity is the point. And the best part is—well, actually there are two best parts—more enjoyment and more consistency. That’s how results stick.