Beyond the Scale: How Bariatric Surgery Improves Co‑morbidities
For adults living with obesity and stacked co-morbidities—type 2 diabetes, stubborn blood pressure, sleep apnea that steals your energy, aching joints, fatty liver—this guide is for you. You’ve probably tried diets, meds, even CPAP tweaks, and you’re tired of chasing numbers that never stabilize. You want real health improvement after weight loss surgery, not just a smaller number on the scale. Learn more about weight loss maintenance. Our bariatric team supports patients through evidence-based surgery, medication integration, and a structured aftercare program that targets remission, medication reduction, and measurable metabolic wins—so you’re not guessing if it’s working, you’re seeing it (in labs, in energy, in life). Learn more about structured aftercare program.
So here’s the thing about bariatric surgery benefits: the weight loss is only part of the story. The bigger upside is metabolic—hormonal shifts that kick fast, sometimes within days. I’ve seen patients drop insulin doses by 50% in the first week post-bypass. Not a promise, just what often happens when physiology turns in your favor.
Look, your goals likely go beyond jeans size. You want diabetes remission, blood pressure control, fewer meds, maybe to ditch the CPAP (safely), and to keep up with kids, grandkids, or a demanding job without crashing by 2 p.m. Let’s map what actually improves, how quickly, and what you can do to lock in those gains. Learn more about sustaining health improvements.
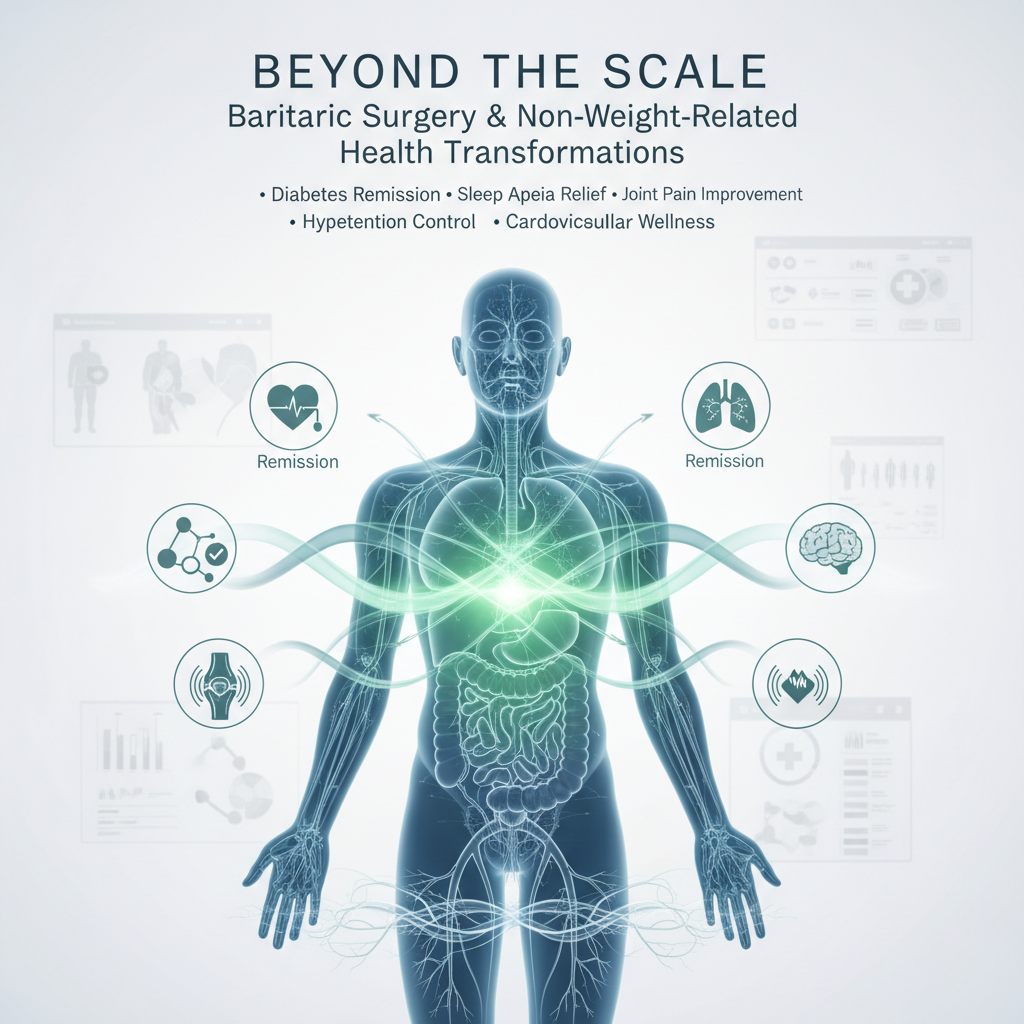
What health conditions improve after bariatric surgery?
Short answer: a lot. And not just “a bit.” Multiple co-morbidities improve—often dramatically—after gastric bypass, sleeve gastrectomy, or duodenal switch/SADI. Here’s the high-level view.
- Type 2 diabetes: Diabetes remission (A1c <6.5% without meds) in many patients; major reductions in insulin and oral meds are common.
- High blood pressure: Better blood pressure control with fewer medications; remission in a substantial portion of patients.
- Obstructive sleep apnea: Significant improvement in apnea-hypopnea index (AHI) and symptom relief; many patients reduce or stop CPAP after medical clearance.
- Dyslipidemia: LDL and triglycerides drop; HDL rises—cardiovascular risk moves in the right direction.
- Nonalcoholic fatty liver disease (NAFLD/NASH): Reduced liver fat and inflammation; fibrosis stabilization or improvement.
- GERD (heartburn): Often improves with gastric bypass; sleeve can worsen reflux for some—procedure choice matters.
- Joint pain and osteoarthritis: Less load on knees/hips, better function, fewer pain meds.
- PCOS and fertility: More regular cycles, improved ovulation and fertility, reduced hirsutism/acne.
- Cardiovascular risk: Lower risk of heart attack and stroke; all-cause mortality reduction over time.
How does bariatric surgery improve diabetes?
Why does diabetes improve so fast? Because gut hormones flip. GLP‑1, PYY, and changes in bile acids and microbiome increase insulin sensitivity and insulin secretion—long before major weight loss happens. That’s the secret sauce.
What’s the typical diabetes remission rate?
It varies by procedure and baseline factors. In broad strokes:
- Gastric bypass (RYGB): High probability of diabetes remission—many programs see 60–80% remission by 2 years, especially if diabetes duration is shorter and insulin need was lower.
- Sleeve gastrectomy (SG): Strong improvement; remission in a meaningful share of patients, though generally a bit less than bypass.
- Duodenal switch/SADI: Often highest remission odds due to powerful metabolic effects, typically used for higher BMIs or severe metabolic disease.
Factors that favor remission: diabetes duration under 5–8 years, A1c not sky-high at baseline, fewer diabetes meds pre-op, and strong adherence post-op.
How fast do meds change after surgery?
Sometimes immediately. Insulin doses often drop in the hospital, then again in the first 7–14 days. Metformin is frequently continued early (it’s kidney-safe for many and supports insulin sensitivity) and tapered later if A1c stabilizes. Sulfonylureas and mealtime insulin are usually the first to go to prevent lows.
We coordinate with endocrinology to write a clear taper plan—because hypoglycemia is real, and success isn’t about being “brave,” it’s about being balanced.
Does bariatric surgery lower blood pressure and cardiovascular risk?
Yes. And the impact shows up both in daily readings and in outcomes that actually matter—heart attack, stroke, heart failure risk. Blood pressure reduction often begins within weeks as vascular resistance and inflammation fall.
What kind of blood pressure control can I expect?
Many patients see systolic blood pressure drop by 10–20 mmHg over months, with medication reduction in parallel. Some achieve remission (no meds, normal BP), especially after gastric bypass. Sleep apnea improvement helps too, because untreated apnea spikes nighttime blood pressure.
What about cholesterol and triglycerides?
Triglycerides tend to fall quickly, LDL improves, and HDL rises over 6–12 months. That combination reduces atherosclerosis risk. In my experience, statin doses are frequently lowered—don’t stop on your own, but do plan for a structured review around 3, 6, and 12 months.
Is sleep apnea cured after bariatric surgery?
“Cure” is the word people search. Real talk: obstructive sleep apnea often improves a lot—and sometimes resolves—but it’s not guaranteed for everyone. Fat distribution, airway anatomy, and residual weight matter.
How soon can I stop my CPAP?
Not immediately. Most programs keep CPAP in place through early recovery because airway swelling and anesthesia can worsen apnea transiently. The safe path:
- Keep using CPAP post-op (it protects your oxygen and heart).
- Reassess at 3–6 months with a repeat sleep study or home sleep test.
- If your AHI is normal and you feel great, your sleep physician may recommend a trial off CPAP.
I’ve seen patients go from an AHI of 42 to 7 by month 6, and then to 3 by month 12. That’s life-changing sleep.
Can bariatric surgery reverse fatty liver (NAFLD/NASH)?
Yes—this is one of the most underrated bariatric surgery benefits. Liver fat often melts quickly with metabolic surgery and protein-forward nutrition.
- Steatosis (fat in the liver): Frequently regresses or resolves within 6–12 months.
- Inflammation (NASH): Many patients improve; some achieve resolution.
- Fibrosis: Stabilizes or improves in a share of patients—earlier intervention tends to do better.
We track ALT/AST, GGT, and non-invasive fibrosis scores. You should see those numbers shift in the right direction as weight and insulin resistance improve.
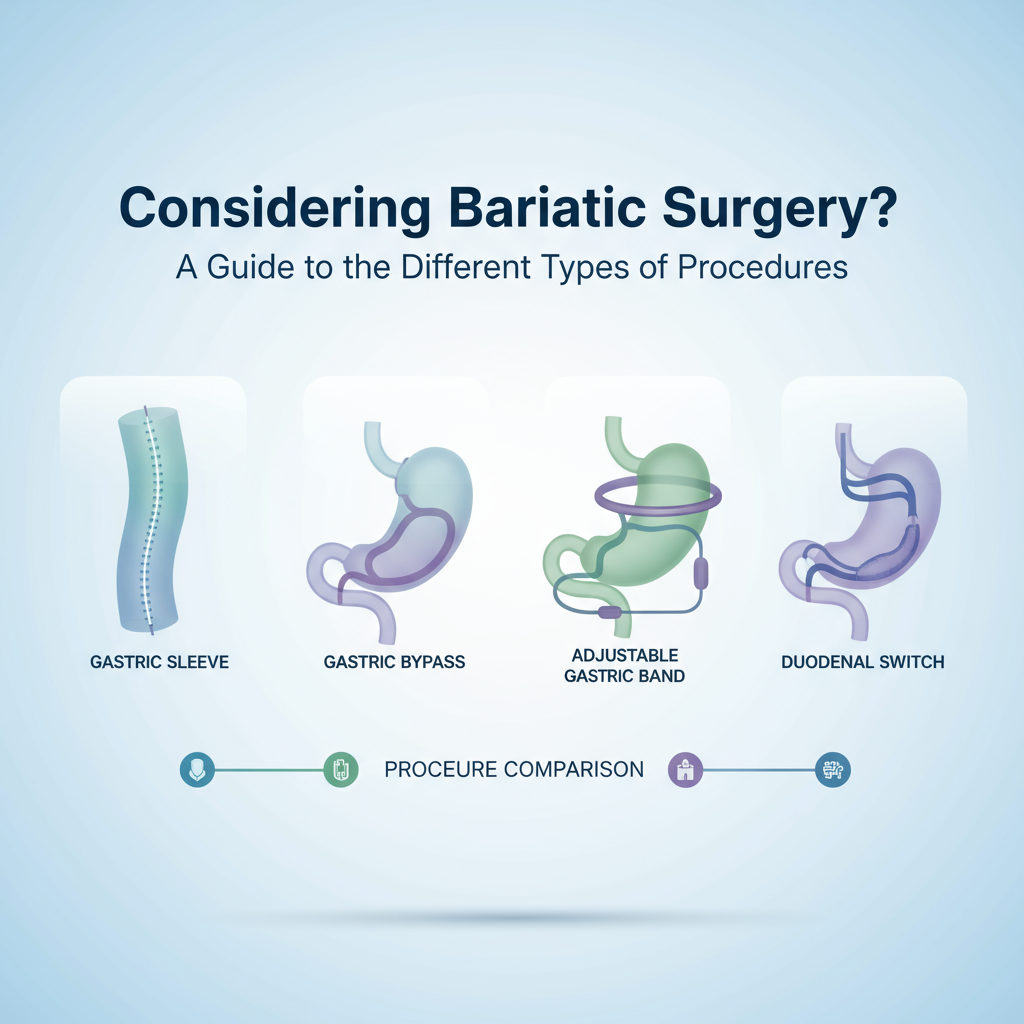
Which bariatric procedure is best for co‑morbidities?
There’s no one-size-fits-all; it’s like choosing between a Ferrari and a bicycle for city traffic—context matters. Still, patterns are consistent:
- Gastric bypass (RYGB): Often the strongest balance of weight loss and metabolic improvement. Great for diabetes remission, GERD relief, and cardiovascular risk.
- Sleeve gastrectomy (SG): Simpler anatomy, strong weight loss and metabolic gains, but can worsen reflux. Good choice for many, especially if reflux is minimal.
- Duodenal switch/SADI: Highest average weight loss and metabolic effect; more vitamin/mineral supplementation and follow-up required.
If reflux is brutal, bypass usually wins. If you need maximal diabetes impact, bypass or SADI tends to beat sleeve. If your BMI is very high or metabolic disease is severe, SADI/DS may be discussed. We walk through risks, trade-offs, and your priorities before deciding together.
What improvements happen when? A simple timeline
Everyone’s course is different, but here’s a practical snapshot I share in clinic.
- Days 1–7: Glucose levels drop; insulin needs fall. Blood pressure begins to ease. You’re tired (normal), but hydration and protein push things forward.
- Weeks 2–4: Energy returns as you hit protein goals. Less edema, improved fasting sugars, lighter CPAP pressures feel easier.
- Months 2–3: Medication reviews. BP meds often reduced. Diabetes meds pared back or stopped if A1c and readings support it. GERD typically better after bypass.
- Months 4–6: Sleep study reassessment for apnea. Lipids shifting nicely. Joint pain noticeably better because you’ve dropped 30–60 pounds by now.
- Months 7–12: A1c can be in remission territory. Liver enzymes normalize. Fitness capacity up—stairs don’t feel like Everest.
- Year 2 and beyond: Maintenance mode. Labs stable, meds minimized, focus on habits and micronutrient health.
Do newer weight-loss meds still have a role after surgery?
Yes. GLP‑1 and GIP/GLP‑1 medications (think semaglutide, tirzepatide) can complement surgery. We use them to:
- Pre-optimize glucose and liver health before surgery.
- Support additional weight loss if a plateau appears.
- Assist with diabetes control in hard-to-remit cases.
It’s not meds versus surgery—it’s a toolkit. The physiology is synergistic, and the “right tool, right time” approach wins.
What lifestyle changes lock in the health improvements?
Weight loss surgery changes physiology; your habits make those changes durable. The best part is—well, actually there are two best parts—your hunger signals are tamer and small consistent actions go further.
- Protein first: Aim ~80–120 grams daily depending on your plan. Protein supports muscle, satiety, and glucose control.
- Hydration strategy: 64 ounces total, sip-by-sip. Separate liquids from meals to protect your pouch/sleeve.
- Plants and fiber: Non-starchy veggies early, then gradual fruit/whole grains per tolerance.
- Movement: Start walking day 1, then 150 minutes weekly by Month 2–3, plus 2–3 strength sessions. Muscle is metabolic insurance.
- Sleep: 7–9 hours; keep CPAP until cleared. Poor sleep sabotages glucose and cravings.
- Micronutrients: Daily multivitamin with iron (if indicated), calcium citrate with D, B12, and others as your team prescribes. Lifelong, not optional.
- Alcohol caution: Faster absorption post-op. Many choose to avoid it, especially year 1.
- Follow-up cadence: Visits at 2 weeks, 6 weeks, 3, 6, 9, 12 months, then annually, with labs.
Risks and trade-offs you should know (and plan for)
No magic wands—just smart risk management. Here’s the straight talk we give every patient.
- Nutrient deficiencies: Risk is real without daily vitamins and labs. Iron, B12, folate, calcium, vitamin D, thiamine—stay ahead of it.
- Dumping or reactive hypoglycemia (bypass): Sugary foods can cause palpitations, dizziness, or late low blood sugar. Balanced meals and protein help.
- GERD: Bypass tends to improve; sleeve can worsen for some. Procedure choice matters.
- Gallstones: Rapid weight loss increases risk; we sometimes prescribe ursodiol for 6 months.
- Loose skin: Common after large weight loss. Compression, strength training, and, if you choose, body contouring later.
- Weight regain risk: Physiologic drift happens. Coaching, meds, and lab-guided tweaks keep you on track.
How we measure success beyond the scale
This is important. Really important. The scale is one metric; your health dashboard is bigger.
- A1c and fasting glucose: Are you trending toward diabetes remission?
- Blood pressure log: Home averages dropping? Meds reduced?
- Lipids: Triglycerides down, HDL up—cardio risk improving?
- Liver markers: ALT/AST normalizing? Fibrosis score steady or improving?
- Sleep: AHI on post-op study, daytime energy, CPAP needs changing?
- Inflammation: hs-CRP lower, joints less painful, mobility up?
- Quality of life: Stairs, travel, work days, sex life—yes, we ask, because it matters.
- Medication inventory: How many bottles did we remove from your shelf?
What a realistic transformation can look like (composite example)
Let’s say Alex, 47, BMI 42, A1c 8.7%, on metformin + basal insulin 42 units nightly, lisinopril 20 mg, atorvastatin 40 mg, CPAP for AHI 31.
- 2 weeks post-bypass: Insulin down to 18 units with fasting sugars 95–115. BP 128/78. Energy “not great but better.”
- 3 months: Down 54 pounds. A1c 6.1%. Off insulin, metformin continued. Lisinopril cut to 10 mg. Triglycerides from 282 to 148.
- 6 months: AHI retest at 8 (moderate), CPAP pressure lowered. ALT normal. Walking 7,000–9,000 steps most days.
- 12 months: A1c 5.5% off meds—diabetes remission. Lisinopril discontinued after home BP average 118/72. Sleep study AHI 3—trial off CPAP with sleep doc approval.
Is every case this neat? No. But with coaching and consistent follow-up, the trend line looks a lot like this. That’s the point.
How our bariatric program supports co‑morbidity improvement
If this feels overwhelming, our team can handle the details while you focus on recovery. Here’s how we stack the deck in your favor:
- Pre-op optimization: Diabetes and BP tune-up, sleep apnea plan, liver-friendly nutrition.
- Procedure selection: We match your co-morbidities and reflux profile to the most appropriate surgery.
- Medication taper protocols: Clear algorithms for insulin, sulfonylureas, BP meds, and statins—safety first, then simplification.
- Integrated GLP‑1 strategy: We use anti-obesity meds when they add value, pre or post-op.
- Nutrition + movement coaching: Protein targets, shopping lists, strength plan you can actually do.
- Sleep medicine partnership: CPAP management and objective reassessment before any changes.
- Data-driven follow-up: Labs at defined intervals, dashboards that show progress beyond the scale.
Quick answers to common search questions
What are the top bariatric surgery benefits beyond weight loss?
Improved diabetes control or remission, better blood pressure control with fewer meds, lower cholesterol and triglycerides, significant sleep apnea improvement, fatty liver reversal, joint pain relief, and reduced cardiovascular risk. People also report better energy, mobility, and mental health.
How fast can diabetes remission happen after weight loss surgery?
Insulin needs can drop within days, with A1c moving toward remission over 3–12 months. Bypass tends to act faster than sleeve. Your baseline diabetes duration and med list shape the timeline.
Will bariatric surgery cure sleep apnea?
It often improves substantially and may resolve, but not for everyone. Plan on a repeat sleep study around 3–6 months and keep CPAP until your sleep physician clears you.
Does weight loss surgery lower blood pressure?
Yes. Many patients see 10–20 mmHg improvements and reduce or stop medications over months. Monitoring at home plus clinic reviews guides safe tapering.
Which weight loss surgery is best for diabetes remission?
Gastric bypass and duodenal switch/SADI generally offer the strongest diabetes remission effects; sleeve helps too. The “best” choice depends on your reflux, BMI, health profile, and goals—decide with your surgeon.
FAQ
How do I know if I’m a candidate for bariatric surgery?
Typical criteria include BMI ≥40, or BMI ≥35 with co-morbidities like diabetes, hypertension, or sleep apnea. A comprehensive evaluation confirms candidacy and selects the right procedure for your health profile.
Can I stop my medications right after surgery?
Don’t stop on your own. Some meds are reduced immediately (like insulin), others later. We create a taper plan based on your readings and labs to keep things safe.
What lab tests are monitored after surgery?
A1c, fasting glucose, lipid panel, liver enzymes, vitamin levels (iron, B12, D, calcium, folate, thiamine), kidney function, and sometimes CRP or ferritin. Frequency is highest in year 1, then annually.
Will I need vitamins for life?
Yes. Bariatric surgery changes how you absorb nutrients. A daily bariatric multivitamin, calcium citrate with vitamin D, and B12 are standard; your team adjusts based on labs.
What if weight plateaus or I regain some?
It happens. We audit nutrition, sleep, stress, and movement, then add tools—structured strength training, GLP‑1/GIP medications if indicated, and refresher coaching. Early tweaks prevent long-term drift.
If you’re ready to trade scale anxiety for real health metrics—A1c in range, blood pressure under control, better sleep, and more energy—our team can help you map the plan, execute the surgery safely, and track every co-morbidity win along the way. Reach out, and let’s get your health moving in the right direction.