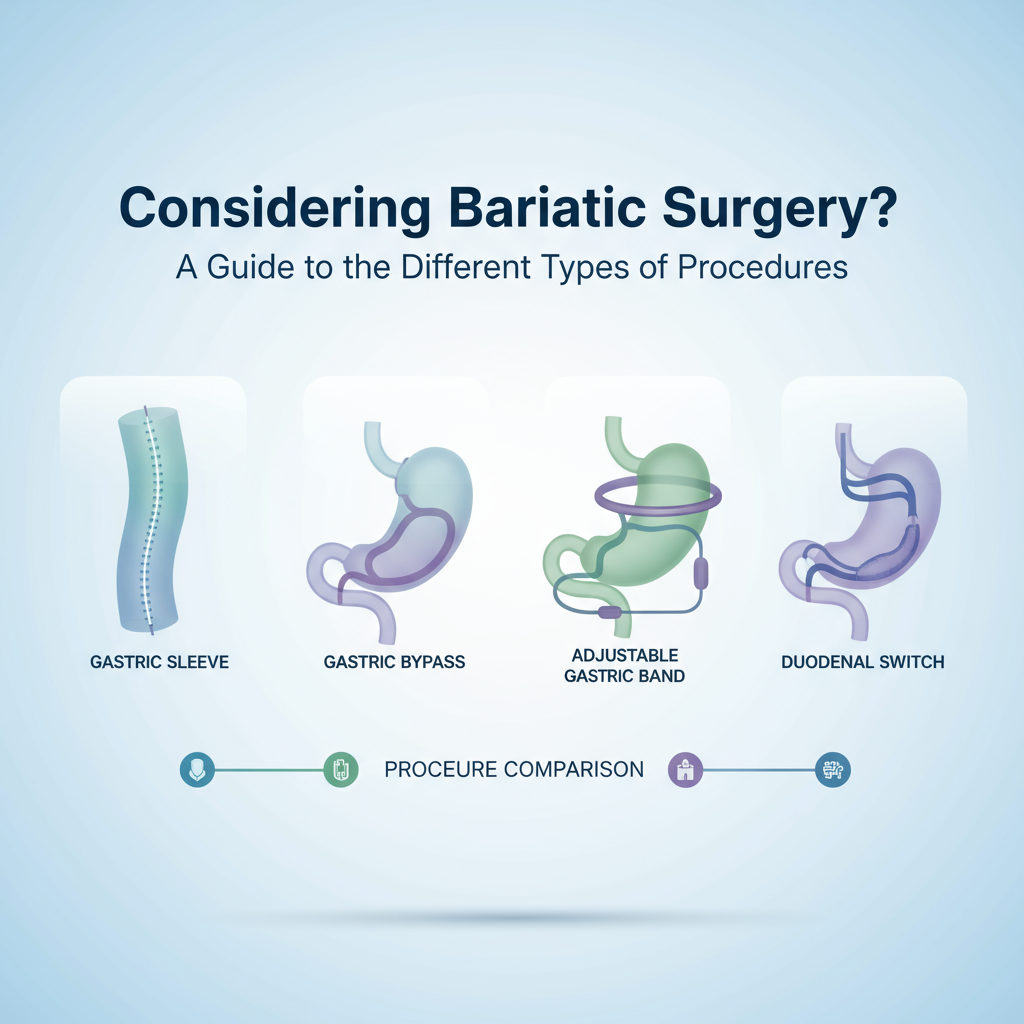
For people who've had bariatric surgery — whether sleeve, Roux-en-Y, or biliopancreatic diversion — and their caregivers, dealing with low energy, hair loss, or confusing supplement lists is stressful and often overwhelming. You worry about malabsorption, which vitamins and minerals to prioritize, and whether your labs or supplements are doing anything at all. Our bariatric nutrition team has managed post-op care for over 12 years and we simplify testing, personalize supplements, and coordinate with your surgeon and PCP so you don't have to guess. Learn more about post-op care.
How do I improve nutrient absorption after bariatric surgery?
Short answer: focus on protein, targeted supplements, timing, and testing. Long answer: you need a plan that covers what you take, when you take it, and how you eat. So here's the thing about absorption - surgery changes anatomy and physiology, and that changes how your body extracts vitamins and minerals from food and pills, plain and simple.
Actionable steps right away:
- Prioritize protein first — aim for 60 grams per day as a baseline, adjust to 60 to 80 grams if your provider recommends more.
- Use a bariatric-specific multivitamin daily (chewable or liquid in the early weeks), then switch to a sustained pill as tolerated.
- Separate calcium and iron by at least 2 hours - calcium blocks iron absorption.
- Take iron with 250 mg vitamin C (or a glass of orange juice) to boost uptake.
- Take fat-soluble vitamins A, D, E, K with a fat-containing meal to improve absorption.
- If oral B12 fails or labs are low, get injectable B12 — many patients need 1000 mcg intramuscular monthly.
From what I've seen, simple timing changes often produce measurable lab improvements within 8 to 12 weeks.
Which vitamins and minerals matter most after bariatric surgery?
There’s a shortlist that shows up again and again. These are the usual suspects you should monitor and supplement.

- Multivitamin: daily bariatric formula with iron for menstruating women.
- Vitamin B12: 350 to 500 mcg oral daily or 1000 mcg IM monthly (many people need injections).
- Iron: 45 to 60 mg elemental for premenopausal women, 18 mg for men and postmenopausal women (adjust to lab results).
- Calcium citrate: 1200 to 1500 mg elemental per day, divided into 2 or 3 doses.
- Vitamin D: 3000 IU daily is commonly used to maintain 25-OH vitamin D above 30 ng/mL (test levels).
- Folate: included in most multis; supplement if low or planning pregnancy.
- Trace minerals: zinc, copper, selenium — check labs and replace if deficiencies appear.
- Thiamine (B1): 50 to 100 mg if severe vomiting or poor intake — deficiency can be acute and serious.
As of 2026, professional guidelines still emphasize lifelong monitoring. So yeah, this is not usually a short-term thing.
How often should I get labs checked?
Routine testing keeps small problems from becoming big ones. Typical schedule:
- Baseline pre-op labs.
- 3 months post-op.
- 6 months post-op.
- 12 months post-op.
- Then annually long-term (more often if symptoms or if you're pregnant).
For iron and B12, many teams test every 3 months for the first year. If you feel new numbness, extreme fatigue, or hair loss, test sooner — don't wait.
What supplements are usually recommended and why?
Here's a practical list and the reason each helps.

- Bariatric multivitamin - baseline coverage for most micronutrients.
- Calcium citrate + vitamin D - bone health and lower risk of osteoporosis.
- Vitamin B12 - prevents anemia and neuropathy, often requires non-oral routes.
- Iron - prevents iron-deficiency anemia (more common after RYGB and in menstruating women).
- Protein powder - helps you reach protein targets without excess volume.
- Trace mineral supplement if labs show low zinc, copper or selenium.
Don't guess on doses. Lab-driven adjustments are the safest route. If you hate swallowing pills, chewables or liquids work early on (chewables are fine long-term if they meet dose needs).

Practical tips to maximize absorption
- Split calcium into two doses during the day - your body absorbs smaller amounts better.
- Avoid coffee, tea, and high-fiber meals within an hour of iron supplements.
- Take fat-soluble vitamins with avocado, yogurt, or a spoon of oil to help uptake.
- If you take a proton pump inhibitor long-term, check B12 periodically (PPI can reduce B12 absorption).
- Address gut issues like chronic diarrhea, small intestine bacterial overgrowth, or pancreatic insufficiency - they all reduce absorption.
Signs of malabsorption - what to watch for
These symptoms should trigger testing or a call to your bariatric team:
- Unexplained fatigue or shortness of breath.
- Hair thinning or brittle nails.
- Easy bruising or bleeding gums.
- Numbness, tingling, or balance problems (neuropathy).
- Bone pain or fractures without major trauma.
- Persistent diarrhea, greasy stools, or weight loss despite adequate intake.
These aren't subtle. If you notice any, get labs and don't try to self-manage with random supplements.
Frequently Asked Questions
Can I stop supplements once I feel better?
No. Most bariatric patients need lifelong supplements. Feeling good doesn't mean stores in your tissues are adequate. Labs tell the real story.
Is food enough if I eat very well?
Food helps, but anatomy changed by surgery often prevents full absorption. Think of diet as necessary but not always sufficient - supplements fill the gaps.
How do I know if I need IV iron or injections?
If oral iron causes GI side effects or labs show severe deficiency despite adherence, IV iron or B12 injections may be required. Your surgeon or bariatric dietitian will advise based on your labs.
If this feels overwhelming, our team can run targeted labs, interpret results, and create a supplement schedule you can stick with (we coordinate with your surgeon and PCP). Call your bariatric clinic, or if you'd like, we can help set up an initial review and a lab checklist to get you started.