For patients who just had bariatric surgery or the caregivers helping them, figuring out which medications to stop, change, or continue can feel scary and confusing — especially with worries about proper dosing, drug absorption, and unexpected side effects during recovery. Our bariatric team helps hundreds of patients every year by reviewing each medication, adjusting forms or doses, and coordinating with your primary care or pharmacy so you don’t have to guess — quietly and safely, while you heal.
How does bariatric surgery affect medication and drug absorption?
Short answer: the stomach and small intestine change, and that changes how drugs get absorbed. Different operations change different parts of the gut, so absorption can fall, rise, or just behave unpredictably.
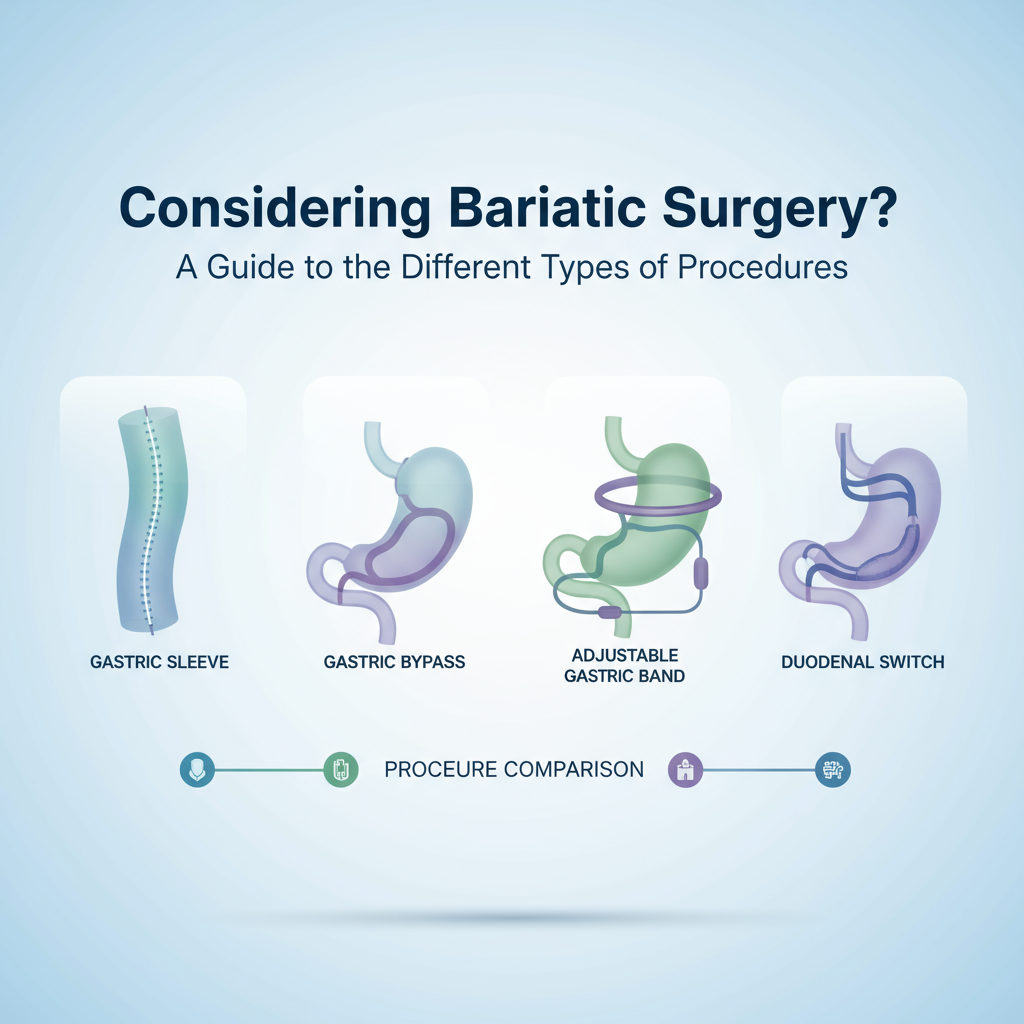
Why? Because many prescription medicines rely on stomach acid, a certain surface area in the small intestine, or slow dissolution to be absorbed properly. After procedures like gastric bypass or sleeve gastrectomy, stomach size shrinks and acid production can drop, and parts of intestine can be bypassed. Learn more about procedures like gastric bypass or sleeve gastrectomy. The result is altered blood levels of pharmaceuticals — sometimes higher, sometimes lower.
I've noticed this clinically: blood levels of antidepressants can dip within 2 weeks after surgery, while pain meds sometimes hit harder because they're absorbed faster (not always). So the usual dose might not equal the usual effect.
Which medicines are most affected after bariatric surgery?
- Extended-release or controlled-release pills — often unreliable (don't crush without checking).
- Oral contraceptives — some types may be less effective after bypass operations.
- Thyroid replacement (levothyroxine) — absorption can change; dosing usually needs retesting.
- Antidepressants and anti-anxiety meds — blood levels can fall, causing reduced benefit.
- Diabetes medications — sometimes need dose reductions fast because blood sugar can drop sharply post-op.
- NSAIDs — risk of ulceration and bleeding; many surgeons recommend avoiding them long-term.
Can I crush pills or switch to liquids after surgery?
Short answer: sometimes yes, sometimes no. You can't assume crushing is safe.
Extended-release tablets are often unsafe to crush because they release the drug slowly over time; crushing them gives a big dose at once and can be dangerous. But many immediate-release pills have liquid or crushable alternatives. There are also transdermal patches and sublingual forms for some drugs.
How to proceed: get a medication review within 48 hours if possible (telehealth is fine). Our pharmacists check which drugs can be crushed, which need blood monitoring, and which should be switched to alternatives. Simple, and it prevents big problems later.
When should dosages be adjusted after surgery?
There’s no one-size-fits-all timeline, but these are common checkpoints:

- Within 48 to 72 hours: pain meds and anti-nausea meds are managed in the hospital.
- By 2 weeks post-op: review chronic meds that affect healing or cause bleeding risk.
- At 6 weeks: repeat lab tests for meds like thyroid, anticonvulsants, or blood thinners if indicated.
- At 12 weeks: reassess long-term meds and vitamin supplementation (many patients need dose tweaks).
So yeah, frequent checks. Not every med changes, but many do. Your surgeon or clinic pharmacist should set these milestones.
What about vitamins, supplements, and interactions with pharmaceuticals?
Vitamins are not optional after most bariatric operations. You're likely to need at least an iron supplement, calcium with vitamin D, and a complete multivitamin — sometimes B12 by injection or sublingual. These help prevent deficiency symptoms that can mimic medication side effects (fatigue, dizziness, brain fog).
Look: some supplements interact with meds. Calcium can interfere with thyroid absorption, iron can bind certain antibiotics, and high-dose vitamin K can affect blood thinners. Tell your providers everything you take — even the herbal tea your neighbor swears by.
Which side effects of medicines should raise alarm bells post-op?
Call your clinic or ER if you have:
- Severe abdominal pain, worsening shortness of breath, or chest pain
- Black or tarry stools (possible internal bleeding)
- Repeated vomiting that prevents taking medications
- Sudden confusion, severe drowsiness, or fainting
- Signs of allergic reaction: hives, swelling, throat tightness
These aren't minor. Get help fast.

How to manage medication safely during recovery - a practical checklist
- Bring a complete medication list to every visit (brand names, doses, and why you take them).
- Ask about switching extended-release to immediate-release or liquid forms if absorption is a concern.
- Request baseline labs for thyroid, drugs that need level monitoring, and complete metabolic panel within 6 weeks.
- Avoid NSAIDs unless explicitly cleared; use acetaminophen and other surgeon-approved alternatives for pain.
- Set up a follow-up with your primary care or specialist within 2 weeks of discharge to coordinate changes.
Who should adjust my medications — surgeon, PCP, or pharmacist?
Short answer: teamwork. Your bariatric surgeon handles immediate surgical risks and medication safety tied to the operation. Your primary care doctor or specialist manages chronic conditions long-term. The pharmacist ties it all together (dose forms, interactions, monitoring plans). Our clinic coordinates all three, which reduces errors. Trust me - splitting care without communication is a common source of mistakes.
Want help? How our team supports medication management
If tracking meds during recovery feels overwhelming, our team does the heavy lifting: we review your list, recommend safe alternatives, write coordination notes to your PCP, and set lab reminders. You get fewer surprises, and more time to focus on healing.
Frequently asked questions
Will my medications always need to change after bariatric surgery?
Not always. Some medications remain stable. But many do need review because of altered drug absorption or changing medical needs after weight loss. Plan on at least one formal medication review.
Can I stop my birth control pill after gastric bypass?
Don't stop it without talking to your provider. Some oral contraceptives may be less effective after certain bariatric procedures; a progestin-only implant or an IUD is often recommended as a reliable option.
Are pain medications more dangerous after surgery?
They can be. Absorption changes may make opioids stronger or weaker. Also, combining opioids with sedating antidepressants or anti-anxiety meds increases risk. Use the lowest effective dose, short courses, and follow your team's plan.
How soon will I need blood tests to check my drug levels?
Typically within 6 weeks for drugs like levothyroxine or certain anticonvulsants. Some meds need checks sooner if symptoms suggest poor control. Your clinic should give you a timeline before discharge.
Who should I call first if I suspect a medication problem?
Call your bariatric clinic during business hours. If it's after hours and you have severe symptoms (breathing trouble, chest pain, severe bleeding), go to the ER or call emergency services.